Key Takeaways
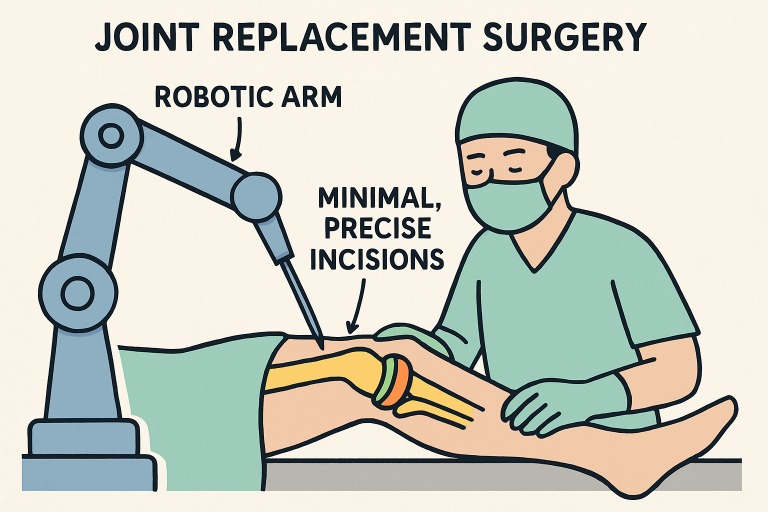
- Robotic-assisted systems enhance the precision and reproducibility of orthopedic surgery, leading to superior implant placement and joint alignment.
- Minimally invasive robotic procedures contribute to reduced surgical trauma and speedier post-surgical recuperation.
- Artificial intelligence is increasingly harnessed to create personalized surgical approaches, optimizing outcomes for individual patients.
- While high upfront investment poses challenges, the sustained benefits drive expanding adoption of robotic orthopedic platforms.
Precision in Joint Replacements
One of the most remarkable breakthroughs in joint replacement is the innovations in orthopedic surgery with MAKO robotics. Systems like MAKO Robotic-Arm Assisted Technology allow surgeons to achieve unprecedented precision in implant placement through detailed preoperative 3D modeling of each patient’s unique anatomy. These robotic platforms enable meticulous planning and execution, ensuring that every cut and prosthetic orientation aligns perfectly with the surgical plan. Real-time feedback enhances soft tissue balancing, reduces the risk of implant misalignment or loosening, and promotes long-term joint stability. Patients benefit from faster recovery, less pain, and minimal tissue trauma, thanks to the fine control afforded by robotic arms. Beyond immediate outcomes, these innovations contribute to longer-lasting implants and decrease the likelihood of revision surgeries, offering a transformative step forward in patient-centered orthopedic care.
Minimally Invasive Spinal Surgeries
Robotics is also having a profound effect on the field of spinal surgery, where precision and safety are paramount. Traditionally, spine procedures were associated with extensive incisions, substantial muscle and tissue disruption, and protracted recovery periods. Thanks to breakthroughs such as the Mazor X and ExcelsiusGPS robots—both equipped with real-time, image-guided navigation—these risks have been significantly reduced. Today, surgeons can perform incredibly complex tasks, like the insertion of screws and placement of hardware, with accuracy down to fractions of a millimeter. The systems use intraoperative imaging to track surgical tools in three dimensions, minimizing exposure to nearby nerves and blood vessels. The result is a greatly reduced impact on surrounding tissue, which translates to less blood loss, lower postoperative pain, and a lower risk of infection or complications.
These minimally invasive approaches also enable patients to leave the hospital sooner and return to their normal routines, contributing to higher overall satisfaction and an improved quality of life. The speed of the patient’s recovery and the degree of tissue preservation are two strong indicators that robotics is reshaping not only how successful a procedure is, but how quickly and comfortably a patient can expect to return to their daily activities. As hospitals and surgical centers continue to embrace robotic assistance, these benefits are becoming increasingly accessible to patients everywhere, offering new levels of safety and predictability in spinal care.
AI Integration for Personalized Surgery
Artificial intelligence stands at the heart of the next wave of surgical innovation. In the context of robotic orthopedics, AI is used to personalize care by combining a patient’s specific physical characteristics, medical history, and imaging data into highly individualized surgical plans. AI-driven algorithms review CT and MRI scans, analyze a range of biometric data, and recommend the best approach for each unique case. During the operation itself, the integration of real-time feedback systems enables the robot to guide or even correct instrument placement instantaneously if deviations are detected. Machine learning models analyze patient metrics both before and during procedures, predicting poor outcomes and flagging potential complications as they arise. For example, refined algorithms can simulate joint function after surgery, enabling surgeons to make real-time adjustments to enhance implant performance and longevity.
Challenges and Considerations
The integration of robotics in orthopedic surgery offers clear clinical benefits, but it also faces significant challenges. High costs for acquisition, installation, and maintenance limit access, especially for smaller clinics. Surgical teams require extensive training to adapt to new technologies, which can slow adoption. Additionally, regulatory and ethical concerns, such as patient data protection, AI transparency, and defining the role of automated recommendations, necessitate strict standards to ensure safety and accountability. As the use of robotic and AI-assisted systems increases, ongoing studies and expert analysis, such as those summarized by U.S. News & World Report, will play a pivotal role in establishing industry-wide standards and best practices. Continued collaboration between technology developers, surgeons, and regulatory bodies will be essential to overcome these hurdles. With careful implementation, robotics has the potential to redefine patient outcomes and the future of orthopedic care.
Future Prospects
Robotics and AI in orthopedic surgery are advancing rapidly, with AR and VR enhancing surgeons’ ability to visualize and navigate anatomy in real time. Emerging smaller, more affordable robots promise wider access, extending sophisticated surgical care beyond major centers to outpatient and community settings. The integration of robotics, AI, and digital health is set to improve safety, outcomes, and surgical precision, enabling more predictable and effective procedures. Leading publications highlight these innovations as transformative for both surgeons and patients, marking a new era in orthopedic care.
Conclusion
The convergence of robotics, AI, and advanced imaging is transforming orthopedic surgery in unprecedented ways. Innovations such as MAKO Robotic-Arm Assisted Technology and minimally invasive spinal robots have enhanced precision, minimized tissue trauma, and expedited patient recovery, while AI integration enables highly personalized surgical planning and intraoperative guidance. Although challenges remain ranging from high costs and complex training requirements to ethical and regulatory considerations the continued refinement and broader adoption of these technologies promise to make state-of-the-art care increasingly accessible. As robotics, AI, and digital tools continue to evolve, the future of orthopedic surgery is poised to deliver safer, more efficient, and highly individualized treatments, ultimately reshaping both patient outcomes and the standards of surgical excellence.